Treating Hyperthyroidism with Radioactive Iodine Therapy
- Nishant KIDANGAN
- Oct 27, 2022
- 5 min read
By Toby Yu
Homeostasis is the regulation of temperature and chemical balance inside the body. In order to maintain homeostasis, many organs work together to sustain a balance within the body. A few ways homeostasis is maintained include thermoregulation, the excretory system, the respiratory centre, and metabolic regulation. This essay focuses on the role the thyroid gland plays in metabolic regulation and the consequences of thyroid malfunctions. (Barclay, 2018)
The thyroid gland is an endocrine gland found in the neck. Endocrine glands secrete hormones directly into the bloodstream based on the negative feedback it receives. In this case, the hypothalamus detects the low levels of thyroxine in the bloodstream which leads the pituitary gland to produce thyrotropin, a hormone which tells the thyroid gland to release more thyroxine. The thyroid gland takes in iodine in the body and converts it into two hormones: tetraiodothyronine (T4) and triiodothyronine (T3), two types of thyroxine. The purpose of these hormones is to regulate the metabolism of cells in the body. Two common disorders are associated with the thyroid: hypothyroidism and hyperthyroidism. Hyperthyroidism is the least common of the two. Thyroid complications are found mostly in women, and 5% of the population has some type of thyroid dysfunction. (Your thyroid gland, n.d.)

This diagram shows where the thyroid gland is located in the human body, which is in the neck in front of the trachea and larynx. This diagram also shows how an enlarged thyroid would appear, which is one of the symptoms of hyperthyroidism.
(Goiter, n.d.)
Hyperthyroidism happens when the body has an overactive thyroid gland, producing too much tetraiodothyronine (T4) and triiodothyronine (T3). These hormones control how the body’s cells use energy, which in turn regulates metabolism. If left untreated, hyperthyroidism can cause heart diseases, vision loss, brittle bones (osteoporosis), and more. Some of the symptoms of hyperthyroidism include weight loss despite no change in food intake or activity, tachycardia, arrhythmia, palpitations, and anxiety. Causes of hyperthyroidism could be thyroiditis, Plummer’s disease, Graves’ disease, or a history of certain diseases, for example, type 1 diabetes or primary adrenal insufficiency. (Hyperthyroidism (overactive thyroid), n.d.)
There are a few ways that hyperthyroidism can be treated, such as antithyroid drugs which block the thyroid’s ability to produce thyroxine, radioactive iodine which destroys the cells that produce thyroxine, surgery to physically remove the thyroid gland, or beta-blockers which block the effect of thyroxine hormones on the body. The solution of main focus currently is radioactive iodine therapy which is a type of radiotherapy. (American Thyroid Association, n.d.)
In radioactive iodine therapy (RAI), radioactive iodine is used to suppress the thyroid gland. Before beginning RAI therapy, the patient should try to reduce the amount of T3 and T4 they have in their bloodstream with medication or a change of diet, or also through an injection of thyrotropin. This is because RAI therapy is most useful when there is a high-level of thyrotropin (a thyroid-stimulating hormone) in the blood. After this is done for a few weeks, RAI therapy can begin. (American Cancer Society, n.d.) A doctor prescribes the patient radioactive iodine (also known as I-131) which is taken orally either as a pill or a liquid. As the thyroid requires iodine to function, it absorbs the majority of the iodine present in the body. When radioactive iodine is inserted into the body, the thyroid absorbs this radioactive substance, killing the overactive thyroid cells and can even cure goitre and kill thyroid cancer cells. The thyroid will take in most of this radioactive substance, and the remaining radioactive iodine left in the body will be flushed out. (Wisse, 2018)
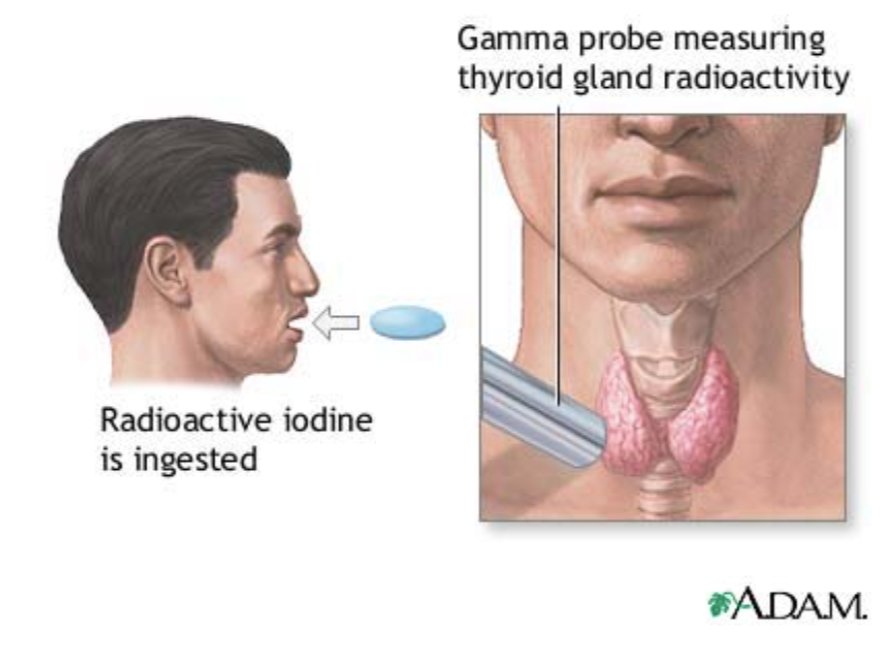
This diagram shows a radioactive iodine pill being ingested. A gamma probe is then used to measure the levels of radioactivity in the thyroid gland to ensure the success of this procedure. (Conaway, 2018)
Radioactive iodine therapy is one of the best choices for patients when it comes to treating hyperthyroidism. This treatment is suitable for the majority of patients, even for those aged 60 and above and children above 5 years old. There is no evidence that the intake of radioactive iodine will cause cancer or other diseases. 70% of patients with hyperthyroidism are treated with RAI therapy as it is seen as the safest long-term solution. When thyroid cells absorb radioactive iodine, they become permanently damaged leaving no chance for hyperthyroidism returning in the future. Patients that choose RAI therapy do not have to be hospitalised as treatment is in the form of a pill, compared to thyroid removal surgery which requires patients to be hospitalised and monitored. It also saves the patient from major complications of going through operations. The patient will be fully awake during the procedure of RAI therapy, unlike thyroid removal surgery, which requires local anaesthesia. People that have gone through RAI therapy will feel almost nothing, and the majority experience no side effects. The body returns to normal days after the therapy as the excess radioactive iodine leaves through urine and saliva. (American Thyroid Association, n.d.)
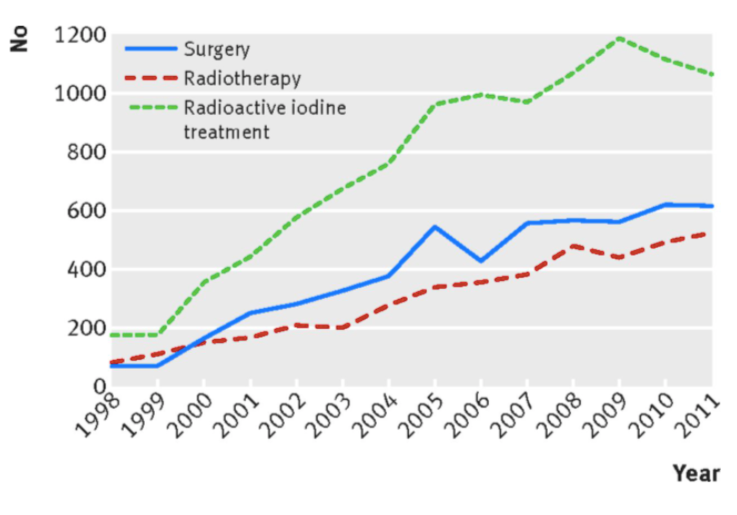
This graph shows how RAI therapy is the most common among treatment methods for hyperthyroidism. (Haymart, 2016)
Even though RAI therapy is safe and has a high success rate, there are a few possible side effects. It is hard to control the amount of radioactive iodine the patient’s thyroid will absorb, so doctors prescribe more than necessary to ensure that the hyperthyroidism is cured. However, this often leads to hypothyroidism - the lack of thyroxine production from the thyroid gland. As the thyroid cells would be permanently damaged by the radioactive iodine, they cannot be recovered to produce more thyroxine again. Instead, the patient will have permanent hypothyroidism. Doctors can prescribe synthetic thyroid hormone pills (usually levothyroxine) to patients who experience hypothyroidism as a side effect of RAI therapy. There are also a few temporary short-term side effects that come with this form of treatment, including swelling in the neck, dry eyes and mouth, temporary tastebuds impairment, and more. Pregnant women also should not receive RAI therapy as this can affect the fetus, and those that have undergone RAI iodine therapy will release radioactive exposure to other people around. (Radioiodine, 2017)

This graph shows the development of hypothyroidism in patients that have undergone RAI therapy as a form of treatment for hyperthyroidism. As shown in the graph, patients can develop hypothyroidism many years after treatment. (Dunn, n.d.)
Thyroid diseases are fairly common and should not be a large concern as they can be easily cured when cared well for. Hyperthyroidism is one of the more uncommon forms of thyroid gland malfunctions, but still, has a range of highly successful treatment options. Radioactive iodine therapy is the most effective and common way to treat hyperthyroidism, and although having both pros and cons to the cure, it is still an important treatment in order to maintain homeostasis within the body.
References
American Cancer Society. (2019, March 14). Radioactive iodine (Radioiodine) therapy for thyroid cancer. Retrieved from https://www.cancer.org/cancer/thyroid-cancer/treating/radioactive-iodine.html
American Thyroid Association. (n.d.). Hyperthyroidism (Overactive). Retrieved from https://www.thyroid.org/hyperthyroidism/
Barclay, T. (2018, July 3). Thyroid and parathyroid glands (S. Curreli, Ed.). Retrieved from https://www.innerbody.com/image/endo04.html
Conaway, B. (2018, February 22). Radioactive iodine uptake. Retrieved from https://www.mountsinai.org/health-library/tests/radioactive-iodine-uptake
Dunn, J. T. (n.d.). Rising Incidence of Hypothyroidism after Radioactive-Iodine Therapy in Thyrotoxicosis. Retrieved from The New England Journal of Medicine website: https://www.nejm.org/doi/full/10.1056/nejm196411122712004
Goiter. (2019, May 2). Retrieved from https://my.clevelandclinic.org/health/diseases/12625-goiter
Haymart, M. R. (2016, July 20). Use of imaging tests after primary treatment of thyroid cancer in the United States: Population based retrospective cohort study evaluating death and recurrence. Retrieved from https://www.bmj.com/content/354/bmj.i3839
Hyperthyroidism (overactive thyroid). (n.d.). Retrieved from https://www.mayoclinic.org/diseases-conditions/hyperthyroidism/symptoms-causes/syc-20373659
Radioiodine (Radioactive Iodine) Therapy: Risks / Benefits. (2017, March 15). Retrieved from https://my.clevelandclinic.org/health/treatments/16477-radioiodine-radioactive-iodine-therapy/risks--benefits
Wisse, B. (2018, October 10). Radioiodine therapy (D. Zieve, Ed.). Retrieved from https://medlineplus.gov/ency/article/007702.htm
Your thyroid gland. (n.d.). Retrieved from British Thyroid Foundation website: https://www.btf-thyroid.org/what-is-thyroid-disorder




Comments